Clinical trials
Evaluation of intraocular implants for presbyopia correction
Presbyopia correction is one of the most challenging tasks in modern cataract surgery. With rising patients expectations not only to improve their vision but also restore the ability to read at far, intermediate and distance without spectacles new IOL models with various optical principles are developed progressively.
Multifocal intraocular lenses (mIOLS) are designed to provide good far and near vision (bifocal IOLs) or even good far, intermediate and near vision (trifocal IOLs) by dividing light in different focuses. The ongoing disadvantage of mIOLs is the loss of quality of vision due to multiple overlapping images of near and distance objects
Rather than creating two or three distinct focal points as multifocal IOLs do, IOLs with extended depth of focus (EDOF IOLs) should provide a wider continuous range of vision, extending the focus from distance into intermediate and even into near range.
Newer IOL models for enhancing intermediate vision are also an approach to partially enable spectacle independency.
We are evaluating various multifocal and EDOF intraocular lens (IOL) designs in respect to visual outcome, optical quality, capsular bag performance and stability as well as side effects in our clinical studies.
Artificial Intelligence in the anterior segment
With the advancement of artificial intelligence (AI), especially deep learning and machine learning, many opportunities have risen in ophthalmology. AI has been shown to be a useful tool in posterior segment diseases such as neovascular age-related macular degeneration or diabetic retinopathy but is also approaching the anterior segment.
The application of AI adds many possibilities to the diagnosis and management of a variety of anterior segment conditions including the use of deep learning to improve IOL Formulas and outsmart existing models.
We are using AI to investigate the anterior segment and incorporate our results into clinical applications such as femtosecond laser–assisted cataract surgery. Furthermore, we are developing an AI based prediction approach for selecting the true IOL dioptric power.
Evaluation of femtosecond laser-assisted cataract surgery
The use of femtosecondlasers (FSL) is increasingly spreading in cataract surgery. Potential advantages over standard manual cataract surgery are the superior precision of corneal incisions and capsular openings as well as the reduction of ultrasound energy for lens nucleus work-up. Specific settings in association with Inflammatory cells during FSL-assisted cataract surgery are being evaluated.
Exact positioning and dimensioning of the anterior capsular opening should help reduce decentration and tilt of the intraocular lens (IOL) optics and thus achieve better target refraction. Additionally, we have the possibility to reduce corneal astigmatism with FSL-assisted arcuate keratotomy during cataract surgery.
Future perspectives of FSL-assisted surgery in the anterior segment include the implementation of primary posterior laser capsulotomy (PPLC). In order to perform PPLC a clear and explicit visualization of the anterior segment including the Berger space is vital.
We are evaluating the efficacy and safety of different surgical prospects in FSL-assisted surgery including the visualization of the anterior segment with the integrated optical coherence device (OCT) of a low-energy FSL device.
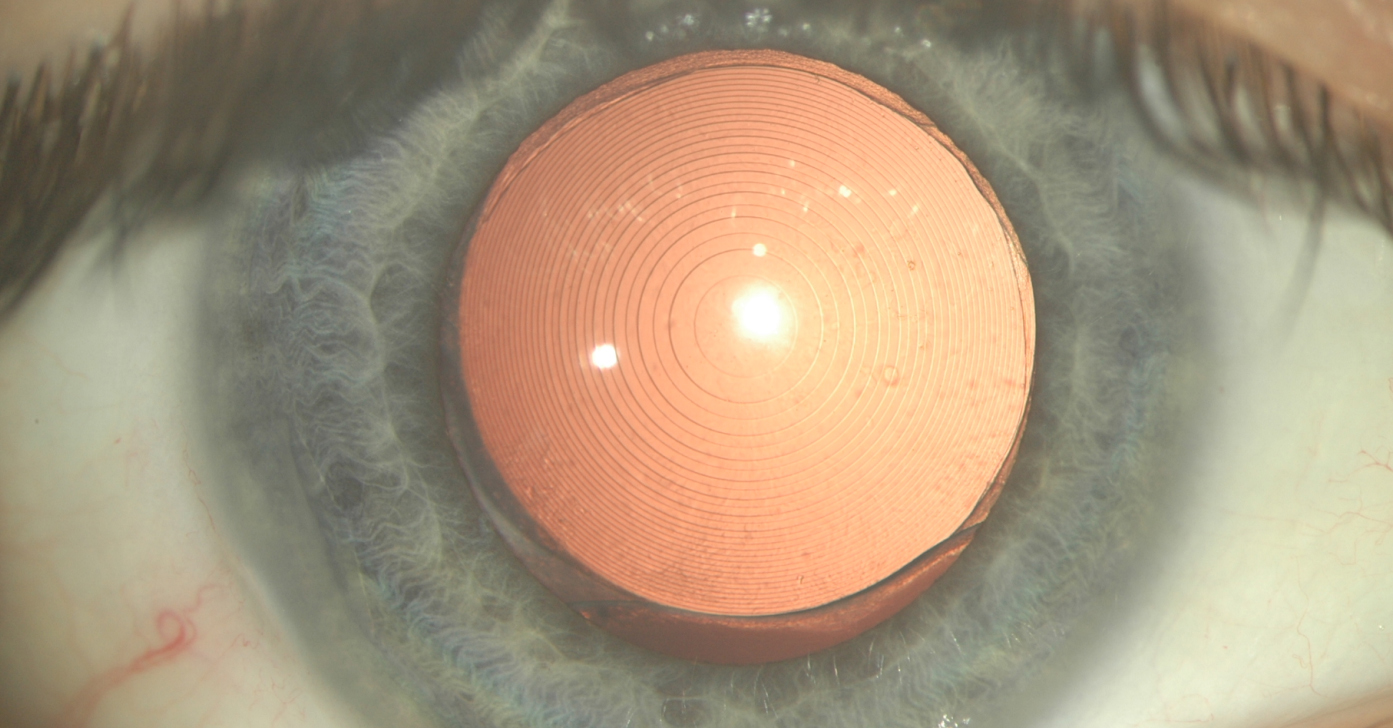
Evaluation of pre-market / post-market toric IOLs
Rotational stability and capsular bag performance are key factors of toric IOLs. Exact evaluation of postoperative rotation is of utmost importance. The Vienna IOL Study Group evolved a standardized study protocol in recent years to evaluate the postoperative stability of IOLs. Baseline measurements are performed at the end of surgery with the patient still supine on the operating table.
The IOLs position will be calculated by comparing the actual IOL axis with episcleral non-movable vessel. This method allows accurate calculation of rotation even within the first critical hour. Postoperative control visits are performed up to 7 months. Retroillumination pictures performed with a customized institutional manufactured coaxial camera allow exact recordings of the IOLs position under full pharmacological dilation of the pupil. Top publications in different journals among the ophthalmic society confirmes the accuracy of our method.
Decentration and tilt measures of the IOLs are performed with a modern anterior segment OCT Casia 2 (Tomey).
Long-term evaluation of intraocular implants
Age-related cataract is the leading cause of impaired vision in the elderly population worldwide. Almost all over 65-year-olds have cataract, 50% notice the visual impairment when they are over 75 years. The only treatment is cataract surgery: the opacified lens is removed and an intraocular lens (IOL) is implanted the capsular bag. In Austria, more than 50,000 cataract operations are performed every year.
Posterior capsule opacification (PCO) leads to a decreased postoperative visual acuity after uncomplicated cataract surgery and is therefore the most common long-term complication. Improvement of surgical methods as well as modification of IOL design and material have led to a lower incidence of PCO nowadays.
Also rotational and axial IOL stability as well as decentration and tilt are important parameters for IOL performance in the capsular bag guaranteeing optimal postoperative vision for the patient.
We are evaluating various intraocular lens (IOL) designs and materials, as well as surgical techniques for the efficient prevention of posterior capsule opacification (PCO) and IOL stability in our clinical studies.
Optimization of preoperative biometry
Several measurements and decisions including biometry, keratometry and IOL power calculation have to be made before surgery. With caution, several pitfalls, resulting in a postoperative refractive error, can be avoided.
Precise and reproducible measurement of the corneal curvature, the keratometry, is decisive for IOL power calculation. Any disturbance of the tear film such as dry eyes or eyedrops can reduce the quality and reproducibility of the measurement of the corneal curvature.
The large number of published formulae lead to confusion. According to the eyes anatomic condition, different formulae shall be used. For clinicians, it is difficult to maintain the overview, which formula to use for which eye. Futhermore, there are various methods to calculate the power and axis of toric IOLs.
We are evaluating not only the keratometric measurement itself, but also consequently the IOL power calculation formulae and toric IOL calculations to improve the refractive outcome.